Researchers in Trinity’s School of Genetics and Microbiology have discovered an innovative new technique of preventing pathogenic bacterial growth. The research focuses on preventative strategies to combat bacterial colonisation of medical devices, such as hip replacements and heart valves, which are to be implanted into the human body. Such strategies could have a direct impact on the recovery of patients undergoing surgical procedures in the immediate aftermath and recovery period.
The discovery consists of a small blocking molecule which prevented “SdrC” staphylocci bacteria from attaching to surfaces and to each other, inhibiting biofilm formation. In laboratory experiments, the blocking molecule, which is a peptide, prevented an SdrC protein from functioning in recognising other bacteria.
This area of research is of particular significance, not only due to the regularity of use of medical devices in modern medicine, but also as a result of recently increased antibiotic resistance, which has become a challenge to safe surgical procedure. Additionally, catheter associated infections in hospitals caused by common skin bacteria such as staphylococcus epidermidis have become ever more prevalent, as some species are now resistant to most available antibiotics.
The use of medical devices to prevent and treat illness and disease is compromised considerably when an accumulation of bacteria adheres to the surface of a device inside the body. Such communities of bacteria are called “biofilms”. These biofilms and the organisms which produce them are areas of intense investigations amongst the researchers in Trinity. Discovering the structure and function of these biofilms allows medical researchers to develop new technologies in response. In addition, biofilm research is undertaken to improve the safety of other common systems, such as the pipes which deliver a domestic water supply.
Species of staphylococci bacteria, strains of which are common and harmless on human skin, can grow on catheters, heart valves, and artificial joints. These communities survive and thrive inside patients because the normal immune defences of the body do not extend to artificially implanted surfaces.
Each incident of biofilm infection costs between €50,000 and €90,000 to the healthcare system, and the patient must usually undergo the surgical removal and replacement of the medical device.
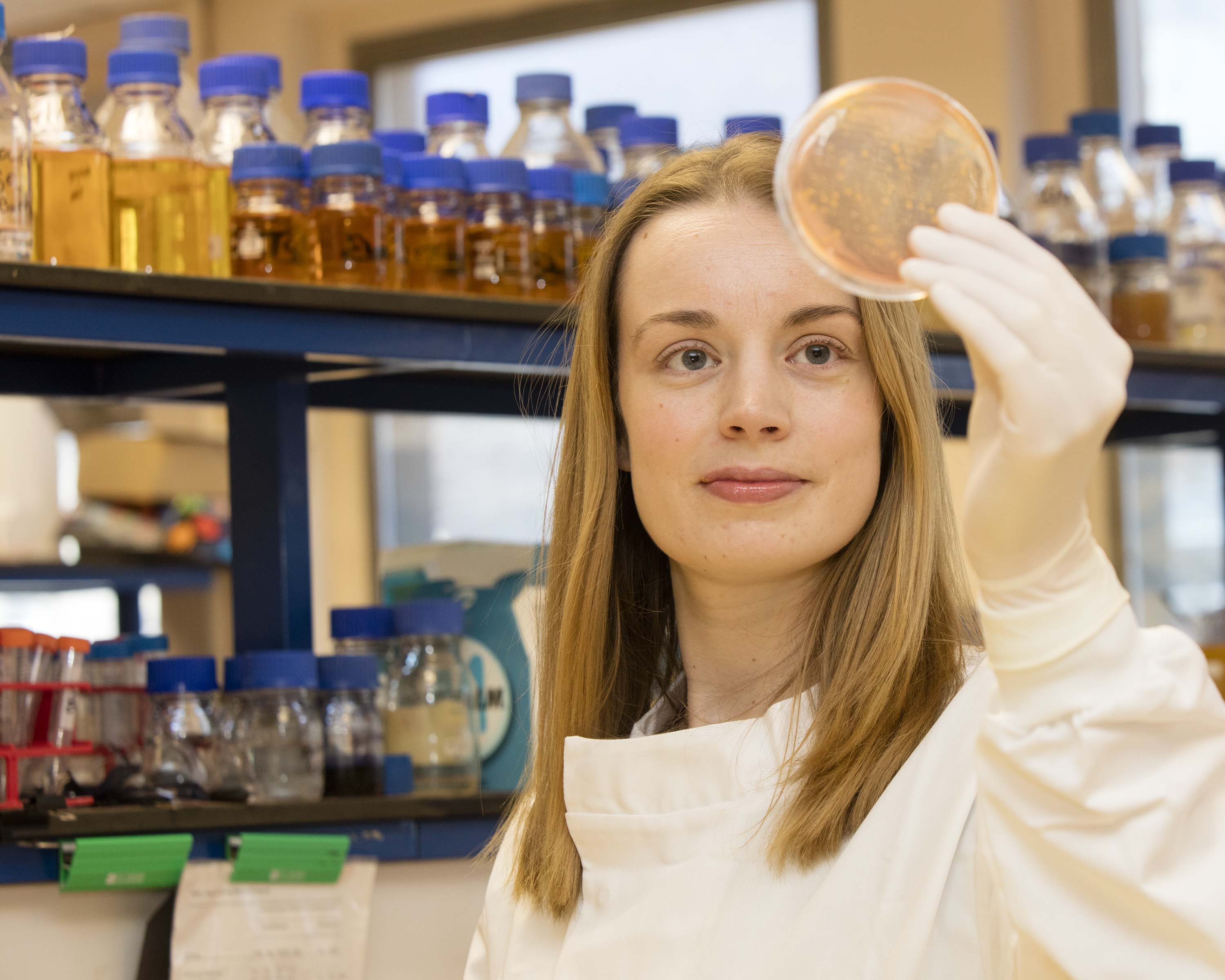
The research team was led by Dr Joan Geoghegan, Assistant Professor of Microbiology at Trinity’s School of Genetics and Microbiology, who is studying new ways to prevent medical device-related infection. A PhD student of the Department of Microbiology, Leanne Hays, worked in collaboration with the atomic force microscopy expert Professor Yves Dufrêne and his team of the Université Catholique de Louvain to make the breakthrough.
Dr Geoghegan said: “These new findings show that it is possible to stop bacteria from building communities using molecules that specifically target proteins attached to the surface of the bacteria. This exciting breakthrough will inform the design of new, targeted approaches to prevent biofilm formation by staphylococci and reduce the incidence of medical device-related infection.“