To assess the failures of the Irish health system, and also to raise awareness for Endometriosis Awareness Month, Trinity News spoke with ten people who all suffer in some way from either endometriosis or PolyCystic Ovarian Syndrome (PCOS). Several of these individuals also suffer from adenomyosis and Crohn’s disease as well as poor mental health due to the neglect of the health systems they’ve experienced for most of their lives.
Endometriosis is a painful disorder in which tissue similar to the tissue that normally lines the inside of the uterus, the endometrium, grows outside the uterus. Endometriosis most commonly involves ovaries, fallopian tubes and the tissue lining the pelvis but can affect the whole body.
Kate, who is a 23-year-old nurse from Dublin, told Trinity News about her experiences with endometriosis. Coming from a family with several women who suffer from the condition, it is surprising that she wasn’t diagnosed until she was 20, but that highlights the complications and failures of the public health system in Ireland. “From when I was 13 I always had horrible period symptoms, extreme cramping, migraines…when I was about 16 this became a major issue as I was regularly being hospitalised due to episodes of pain that would often cause me to faint. I felt like I was never understood and people would constantly tell me it was “normal” to be in pain,” she explained.
Kate spent around four years “in and out of different hospitals” before her diagnosis. “Just about every doctor I spoke to told me I was “too young” to have endometriosis. The one doctor who told me he could put me on a public waiting list for a laparoscopy told me that due to waiting lists I’d likely not get a call until my mid-twenties.” When she turned 20, she was diagnosed with stage 3 endometriosis and told it had progressed badly for someone so young.
As for treatment, Kate was offered hormone replacement therapy (HRT), the Mirena coil or a yearly laparoscopy. “I point-blank refused HRT and accepted the Mirena coil with a view of continuing laparoscopies to have endometriosis burnt off my uterus. I had a horrible experience with the Mirena and had it taken out not long after insertion, to which my gynaecologist informed me he no longer sees how he could treat me and discharged me against my wishes,” Kate recalled.
Kate was also gaslit by her medical practitioners. She explained how last year she made an appointment with a new gynaecologist and had “a nightmare experience.” Kate had the same repeated conversations with him regarding HRT and her preferences and so offered her an alternative of a contraceptive pill for her condition. “While in the hospital car park, the doctor called me and said I wouldn’t have protection on this pill and would still have to use barrier methods. I brought my prescription to my local chemist who told me I wouldn’t be able to use my medical card to cover the cost of the drug and it would be €177 a month.”
“The pharmacist said she was 99% certain the drug I had been prescribed was a form of HRT. I did my own research once home and found out this was true. Since then, I have not sought any treatment for my endometriosis as I feel traumatised from my previous experiences. I now just take standard painkillers to manage it, which is rarely effective.”
“[They did] everything to shift the blame of my pain onto me. Demanding if I was pregnant, did I have STDs? Did I hurt myself with a sex toy, am I getting my ‘holes’ mixed up?”
Jodi, a 21-year-old student, has a similar experience with being treated horribly by staff in an Irish hospital. She explained: “I had a bad experience with nurses and doctors in James’ Hospital Dublin who did not take my pain or symptoms seriously. [They did] everything to shift the blame of my pain onto me. Demanding if I was pregnant, did I have STDs? Did I hurt myself with a sex toy, am I getting my ‘holes’ mixed up?” As a result, she went to Poland earlier this year for treatment: “I travelled to Poland to seek a medical exam. I wanted to go and get seen so badly I didn’t register properly that I was travelling to the other side of Europe for a doctor’s appointment.”
Detailing her treatment abroad, Jodi noted how the appointment was “smooth” and “an overall positive experience”. “I was treated for an infection in my uterus but it still hasn’t gotten me all the answers I need, something like an infection could’ve been so easily treated at home,” she explained.
When asked how endometriosis affects her daily life, Jodi pointed out that she misses days of work, days of college, and that “It’s really starting to have a hugely negative emotional toll on [her] with feelings of anger, frustration, guilt, restlessness, agitation, sadness.” She noted the emotional toll it has had on her: “I never know when a flare-up is coming so I can never prepare for it, the fear that it’s going to come at an inconvenient time makes me incredibly anxious, constantly living on edge of when it’s going to attack,”
“I cannot have painless sex, I cannot wear tight clothes. I have pelvic floor therapy every fortnight. The fear of infertility, along with the unknown, has a huge emotional toll. I go to therapy along with taking 20mg of Lexapro. I would not be able to live without painkillers and I am in constant fear of ovulating or menstruating.”
Lara, a 21-year-old from Navan, Co.Meath also spoke to us about her daily experiences with endometriosis. Currently studying for her Master’s in human resource management in DCU, Lara described how endometriosis affects her in “every way” on a daily basis. “From the moment I wake up in the morning, I feel bladder pain, bowel issues, along with my regular endometriosis pain,” she said. “I cannot have painless sex, I cannot wear tight clothes. I have pelvic floor therapy every fortnight. The fear of infertility, along with the unknown, has a huge emotional toll. I go to therapy along with taking 20mg of Lexapro. I would not be able to live without painkillers and I am in constant fear of ovulating or menstruating.”
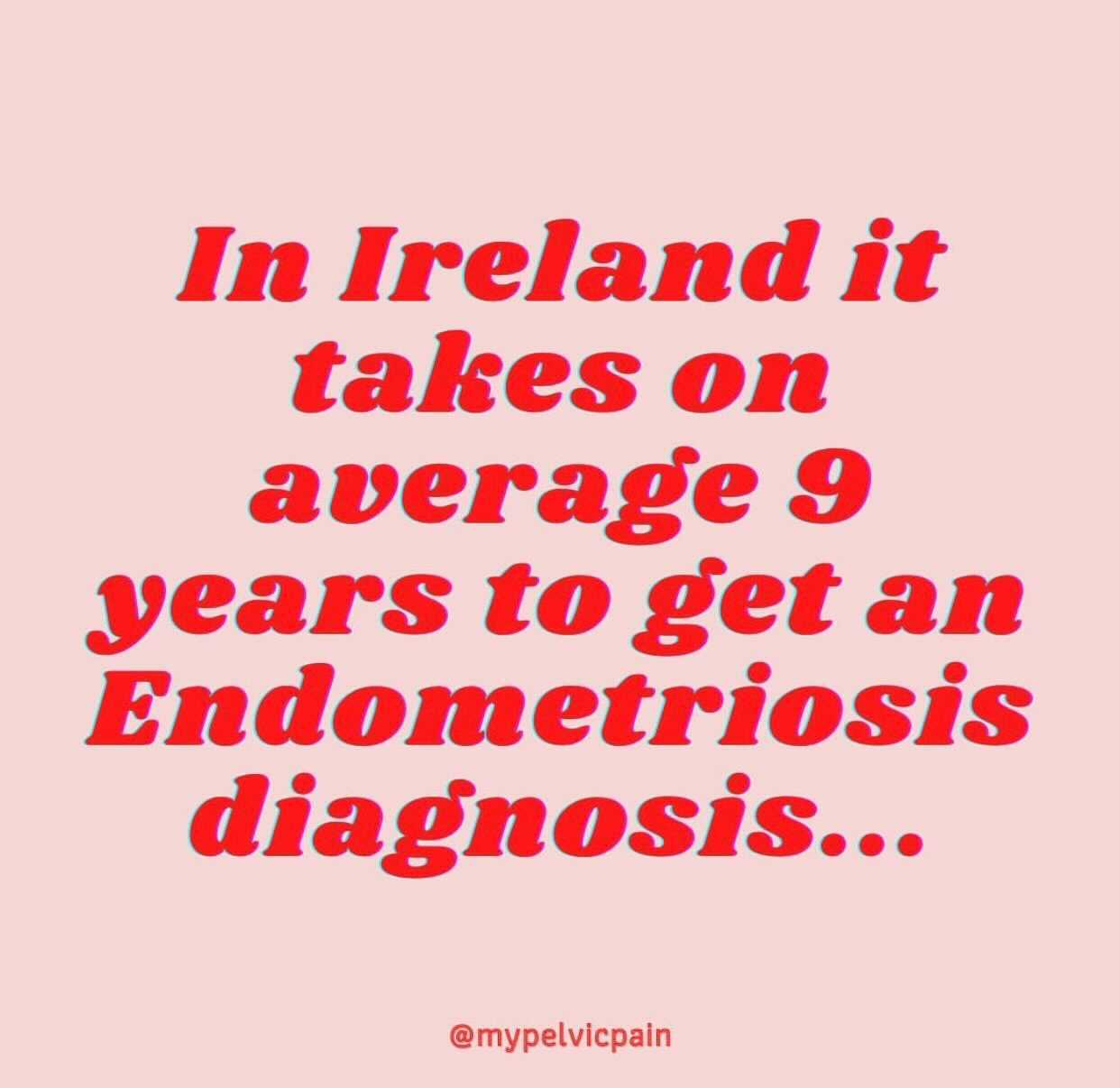
On February 4, RTÉ reported the case of Laura Newell, a 39-year-old woman who died after taking over-the-counter medicines to treat her undiagnosed endometriosis. But instead of focusing on the issue of endometriosis – which takes nine years on average to get a diagnosis in Ireland – TDs in the Dáil discussed the availability of strong painkillers on the internet. When asked about how she felt about the news story, Lara commented that she can “relate to being treated like I was “just looking for painkillers”.
“I am privileged to be prescribed the painkillers that I need, but if I wasn’t, I would not be able to live without them. This is a tragedy for the endometriosis community, as it highlights the mistreatment and lack of education surrounding the disease. If this woman had adequate healthcare, this would not have happened,” she continued. As for improving the system in Ireland, Lara has a few ideas: “Shaming women for needing painkillers or basic healthcare is not normal. It is a chronic disease and needs to be treated as one. I am privileged to be able to access private healthcare and health insurance, but if I had to wait publicly for my treatment, I do not know if I would be here today.”
Polycystic ovary syndrome (PCOS) affects how ovaries function. It can affect hormones, fertility and periods, causing hair loss, chronic pain, internal cysts and weight gain. Polycystic ovaries are very common, approximately affecting 20% of women.
Éabha, a Master’s student from Cork, spoke to Trinity News about her diagnosis journey: “I suppose while I had been noticing symptoms of PCOS since I was 18, I only really started to take these seriously and seek a diagnosis when I was 20. I had started to notice that my hair was thinning a lot, to the point I had two almost bald patches behind my ears. I decided to properly get checked out by a doctor, since Googling my symptoms had freaked me out a bit.”
Éabha noted that “as usual” Google was very wrong but was “surprisingly was more accurate than how the real doctor reacted.” She was told to stay away from Google and everything was once again blamed on stress and her lifestyle. It took until she was 22 to get an ultrasound.
“After many arguments with my doctor, he eventually referred me to the HSE. While I was delighted to get the referral it really felt more like he was doing it to get me off his back rather than out of actual concern for my health,” she explained.
When Éabha received her HSE letter it stated that she was on an 18-month waiting list to be seen. Through a family connection, she was fortunate enough to get a private consultation and a diagnosis but still can’t afford to get a smear test due to the cost. Even after obtaining her official PCOS diagnosis, Éabha has found that medical assistance is incredibly poor: “Upon returning to my previous GP, he never really gave me any advice regarding treating my PCOS. The only advice he did give me was to exercise more and try losing weight. This makes me laugh as if he actually paid attention to my medical files he would have seen that I’m medically underweight.”
When asked what she thinks should be done by the Government to improve PCOS screening measures, Éabha pointed out that accessibility is a major issue. “I think the screening process could definitely be evaluated that every woman in Ireland over the age of 16 should be eligible for a free ultrasound much the same way as every woman over 25 can access smear tests and every woman over 35 can access mammograms,” she said. Éabha also noted that medical staff need to be taught how to show compassion so they “know how to speak to a woman who is being told that she may never be able to have kids, to be able to actually sound empathetic while saying “I’m sorry that your reproductive organs are going to cause you pain for the rest of your life.”
Rachel, a 27-year-old from Meath, told us her story about how her sexuality affected her diagnosis journey and what it was like to seek PCOS treatment abroad. “At 12 I started my first contraceptive pill to help manage the pain. Despite the fact my period reduced me to tears every month and left me lying in bed unable to move, I stopped looking for help. I kept being told that it was normal, that it was part of being a woman,” said Rachel. “When I was 23 I met my now wife, Karen. She rarely needs to even take paracetamol for her period. It was only then I really started to think about the difference in our experiences and started to look into what could be causing my severe period pain.”
Her experience with PCOS has been “long, frustrating, and sometimes absolutely heartbreaking.” “I can’t count how many appointments I had with GPs from the age of 11-25 about my periods,” explained Rachel. “Each time it was just a different combination of painkillers that were recommended. In 2019, when I turned 25 I went for my first smear test and as part of the appointment, I talked about my period history. The doctor listened to everything I had to say and was the first person to tell me that the pain I was experiencing was not normal.”
Rachel described how she was referred to a gynaecologist who scheduled her in for surgery to look for endometriosis. “I ended up being readmitted to the hospital twice after the surgery within two weeks for severe pain. It turned out I had cysts on both ovaries and I had developed an infection after the surgery,” she recalled. After being discharged with dysmenorrhea – “a fancy medical term for painful periods” according to Rachel – she was bed-bound for three months in 2020 due to pain. “I ended up in A&E multiple times over this period due to cyst ruptures. My GP referred me to a gynaecology service and I received a letter to say I was on the urgent list and I would be seen in approximately 56 weeks,” she explained. After seeking private treatment, she finally received her diagnosis of PCOS.
But things didn’t get better for Rachel. In 2021, she still faced multiple A&E visits due to cysts rupturing. Her hospital then suggested a trial of decapeptyl, which induces menopause for a few months. “The reasoning was that it would shut my hormones off and if the pain disappeared or stayed then they could rule out possibilities,” Rachel explained. When she realised she would have to see a gynaecologist again, she specifically requested not to see her initial male doctor as “he had been dismissive previously” and “didn’t take [her] pain seriously.” Despite reassurance that he would not be present, he appeared during the appointment to sign off on her drug trial. He refused to.
“I asked him at what point would a hysterectomy be considered for my pain considering I have tried all of the less invasive options that are recommended. He told me that it would not be an option because of my age. He said I was too young to consider such a drastic decision,” said Rachel. “He said he had never performed a hysterectomy on someone my age and he didn’t plan to do so either. He said that it would be a different conversation if I was 45, but as I’m so young and have 15 plus years left of fertility, he wouldn’t consider it as an option.”
“Word for word he said, “I don’t want you to have regrets if circumstances change for you, maybe you leave your partner, your sexual orientation changes, you meet someone and HE wants children.”
Once Rachel and her wife challenged him further, the reasoning only got worse from there. After explaining to him that she had felt suicidal due to the pain, the consultant then said that he didn’t want Rachel to get a hysterectomy while her judgement was “clouded by the pain”. “Word for word he said, “I don’t want you to have regrets if circumstances change for you, maybe you leave your partner, your sexual orientation changes, you meet someone and HE wants children.” At this point, I knew there was no room to discuss this with him. I had opened up about how bad the pain is and how much it impacts my mental health, but his only concern was for a fictional man who may want me to carry his child in the future,” she recalled.
Soon after this, Rachel was admitted to A&E again. The doctor gave her ten days’ worth of codeine and warned her to only come back if she showed signs of sepsis as it “wasn’t the place for chronic conditions.”
Rachel recalled the moment she gave up on Ireland’s healthcare system: “ I asked her what I should do if the pain doesn’t go away and she told me to speak to my GP about getting a referral to a pain clinic for ketamine injections to manage the pain. At that point I gave up on Ireland being able to give me proper reproductive healthcare.”
Christine, who was born in Limerick but has now relocated to Scotland, highlighted the lack of care and affordable treatment options for those with PCOS when telling their story.
Christine explained how “there’s a relief in receiving a diagnosis” but “as a lesbian, being on the pill is an unnecessary convenience”. The increased risk of blood clots and diabetes as a result of the contraceptive pill is an issue that is often brushed under the carpet. Looking at the backlash from the possibility of blood clots with the Astra-Zeneca vaccine, it is infuriating to realise that the general public simply doesn’t care enough about reproductive health. Christine also noted the cost of the pill as a treatment”, and said “it should be free” as a result. According to Christine, there is a “lack of knowledge and an insistence that period pain and irregular cycles are normal when severe cramps never are ” which contributes to misdiagnosing of these conditions.
Kitty, 24 and from Limerick, has also recently relocated to Scotland. They expressed their frustration at the Irish healthcare system as when they were 17, a doctor had found high testosterone levels in their blood, which was caused by PCOS. Kitty discussed how the Scottish system is much preferable to the Irish one as medical appointments are free. “I used to be paying €90 for my medications, plus €60 for my doctor’s visits and an extra €30 for any blood tests or examinations,” Kitty explained.
When asked what they are most angry about when it comes to the treatment of people with reproductive issues in Ireland, Kitty pointed to the fact that these disorders are “so overlooked despite being so common.”
“It got ignored by my first doctor, I was never taught anything about it in school, the information I did find is incomplete or dangerous regarding diets and fertility because we’re made to rely on word of mouth online, and a lot of wellness bloggers exploit that in my opinion. A lot of the information out there is misleading or downright dangerous. I came across so many wellness blogs pushing for people with PCOS to stick to a strict keto diet, to cut out all sugars, basically saying if you eat white bread or anything fried then you’re 100% gonna become diabetic,” Kitty explained.
“That makes me really angry because I’ve struggled with an eating disorder for most of my life and a lot of people with PCOS do, so for wellness bloggers to advise such strict food exclusions is very dangerous.”
Several of those who came forward to tell their stories for this article suffer from multiple disorders as well as endometriosis or PCOS. Danielle, a speech and language therapist, told us about her experiences with endometriosis, PCOS and adenomyosis. She recalled when she was a teenager, she “was asked by a doctor if I discussed my periods with my friends. I was 15 at the time and so embarrassed by this. I answered no and the doctor responded by asking how I knew my periods were so bad if I wasn’t comparing them to others.”
Danielle travelled to the UK in 2020 in order to receive excision surgery which is comparable to “taking the weed out by the root- it takes longer for the weed to grow back and doesn’t in some instances.” When asked what she wishes people would know about her conditions, she said: “That there is no cure. Endometriosis is not the lining of the womb but cells similar to the lining of the womb. The definition is so important as it gives reason as to why medically stopping the lining of the womb from growing doesn’t halt the growth of endometriosis. A hysterectomy will not cure endometriosis. Endometriosis is a whole-body disease.”
She explained that she feels that health issues that just happen to be associated with reproductive organs aren’t seen as medical issues: “I have bowel endometriosis and have seen a dietician and now eat a gluten-free diet to try and manage the bowel symptoms I experience due to the damage endometriosis has done to my bowel. What is the pill going to do for that?”
“I would have done anything to be able to function like a normal teenage girl. I tried my best but sometimes it was hard. I found it hard to talk about this because I was under the illusion that you don’t talk about women’s health issues”
Sarah Jane, a 28-year-old media coordinator at Web Summit, also came forward to tell her story about suffering from PCOS, endometriosis and adenomyosis. She became aware of her chronic pain at the age of 8: “From the age of 8 up until I was 23, I was in and out of A&E as I was always struggling with the pain. But every time I went into the hospital, I was dismissed. I was told it was rumbling appendix, IBS, that I’m not clearing my bowels properly, that I was looking for attention or the worse of all – it’s just period pain.”
She described how as a teenager, she missed so much school that the Department of Education sent an officer to her house to see if she really was sick. “I would have done anything to be able to function like a normal teenage girl. I tried my best but sometimes it was hard. I found it hard to talk about this because I was under the illusion that you don’t talk about women’s health issues,” Sarah Jane explained.
She now uses her experiences to educate others on what it means to have chronic pain. “I make it my mission to de-stigmatise these issues. I talk about when I get my period on my socials (@sarahjanevlogs), at work, to my friends etc. I talk about every appointment I have and what is going on. I post about what side effects I have and try to educate others on these conditions. I talk so openly about it that the company I work for, Web Summit, asked me to do a talk on my journey with endo, PCOS and adeno to help educate people about these issues.”
Sarah Jane described how nearly all of the good experiences she’s had with her diagnosis journey have been outside of Ireland. “There are three standout moments of horrible experiences that will never leave me. The first one was when one of my Irish gynaecologists told me I was the issue. It’s my fault I can’t be helped – and she was saying this all because I can’t take the pill due to mental health issues as well as suffering from migraines.”
“The second moment was when my second Irish gynaecologist said to me that he didn’t know what to do next for me. He then turned and flippantly said ‘how about we take out your right ovary and see if that helps.’. I broke down into tears. The fact that he wanted to do this without freezing my eggs or couldn’t guarantee this would help was utterly upsetting. He couldn’t understand why this was upsetting either.”
The third stand out moment for Sarah was in August 2020. She had been suffering from pain for almost 10 days and was unable to eat. “A gynaecologist came up to me and looked at my notes and then said “Have you a boyfriend?”, I was confused but I said yes. She then said “Do you want kids?” and I said “Yes, but not for another few years yet, I’m on 26 and just got my dream job” and she turned to me and said “Well, my advice is to play that card and get pregnant, it will cure you,” she said. This was the fifth time Sarah Jane had been told to get pregnant. She sobbed for the rest of the day in the hospital bed.
It took Sarah Jane 14 years to get a diagnosis. She has had 9 surgeries since 2016. She described the severe pain she experiences nearly every day: “Sometimes, when I am in bed at night I can’t move because if I move, this shooting pain will start again; I’ll be sweating, I’ll be putting the pillow in my mouth as to not scream in pain, my chest against my bed, grasping the sheets tightly, tears will be streaming down my face. I’ll take the strongest pain relief I can and watch the clock until I can take my next batch. Sometimes, I try not to breathe too much because that causes the pain to increase. These days, all I can do is make a hot water bottle and tea and get back into bed. Some days I need a walking stick to get from place to place. Sometimes I need a wheelchair because I can’t stand up straight.”
It’s not surprising that word-of-mouth and online activism has become a major support for those who suffer from these disorders. Northern Irish activist and writer Sarah Rose, also known as @mypelvicpain on Instagram, spoke to Trinity News about the misinformation that exists when it comes to these chronic disorders: “There’s no updated knowledge surrounding these conditions. There’s no joining up the dots or the big picture when you’re getting diagnosed.” She also notes that endometriosis is automatically linked to the womb’s lining: “It isn’t the endometrium. It’s not a bad period, it’s not a menstrual disease, it’s a full-body condition. It impacts every organ, including the brain and lungs.”
“When I first considered I had endometriosis, I Googled it and all the information I found was incorrect. I know until recently the NHS had the incorrect definition on their website.”
Her own experiences with chronic pain began before she turned ten. As a teenager, Sarah Rose developed an eating disorder due to the pain. From the age of 18, it took her a decade to get a diagnosis. “I felt like I was losing my mind, I was constantly in A&E, constantly seeking help. I’d wait two years to see somebody just for them to say there’s nothing wrong with me.” If it wasn’t for social media, Sarah Rose wouldn’t have realised that she had endometriosis. “When I first considered I had endo, I Googled it and all the information I found was incorrect. I know until recently the NHS had the incorrect definition on their website,” she explained.
Sarah Rose shares information about her experiences with endometriosis, adenomyosis and Crohn’s on her Instagram page, @mypelvicpain. With over ten thousand followers, she promotes how both the UK and Ireland can reform their healthcare systems to start taking chronic illnesses seriously. When asked what she thinks should be everyday knowledge about these conditions, Sarah Rose pointed out that people are often left suffering for nearly a decade before getting help. Currently in Ireland, it takes on average nine years to get an endometriosis diagnosis. In Northern Ireland, it takes an average of eight and a half. “The one thing that is the most damaging thing about endometriosis is the misinformation,” she explains. “There’s no cure. And people assume that there is. All the “cures” relate to the womb and nothing else. People are also told it can only occur during certain ages so they’re dismissed and forgotten about.”
In order to write this article, I put out the call on my social media. I lost track of all the people who responded to me. A wave of horrific stories and sadness flooded my mentions on Twitter and Instagram. The cost of these issues both emotionally and financially is irreparable. No one should suffer like this.